 I'm going to have a little rant now. Apologies to all!
WHY do our computers still require "mouse marksmanship"? You know the problem: where you have to spend ages waving the cursor around and over a thin line of pixels, until the cursor finally changes to a double-headed arrow, and you can grab and drag the item - perhaps a wall between two panes in a program's window. Or where there are several tightly-packed buttons and, unless you're accurate, you click the wrong one...with disastrous effects?
Touch-screen interfaces are no better. In fact, they're worse, since fingers are even less accurate than mice or trackpads, and - worse still - they obscure the user interface (UI) elements they're supposed to be interacting with!
I mean...seriously...why is this still a thing? We're perfectly capable of designing operating system interfaces, and applications, that can make sensible guesses as to the user's intention. We can create UI elements that don't need this kind of fine movement requirement - frustrating even to regular users; literally impossible for some to use.
"Mouse marksmanship" makes the whole thing hostile to anyone with a hand tremor, anyone with co-ordination issues or some classes of disability, anyone with even moderate visual difficulties - and everyone else, too.
It's just crap. It's decades-old design, inherited from the 1973 Xerox Alto, and we need to get past it.
I'm going to have a little rant now. Apologies to all!
WHY do our computers still require "mouse marksmanship"? You know the problem: where you have to spend ages waving the cursor around and over a thin line of pixels, until the cursor finally changes to a double-headed arrow, and you can grab and drag the item - perhaps a wall between two panes in a program's window. Or where there are several tightly-packed buttons and, unless you're accurate, you click the wrong one...with disastrous effects?
Touch-screen interfaces are no better. In fact, they're worse, since fingers are even less accurate than mice or trackpads, and - worse still - they obscure the user interface (UI) elements they're supposed to be interacting with!
I mean...seriously...why is this still a thing? We're perfectly capable of designing operating system interfaces, and applications, that can make sensible guesses as to the user's intention. We can create UI elements that don't need this kind of fine movement requirement - frustrating even to regular users; literally impossible for some to use.
"Mouse marksmanship" makes the whole thing hostile to anyone with a hand tremor, anyone with co-ordination issues or some classes of disability, anyone with even moderate visual difficulties - and everyone else, too.
It's just crap. It's decades-old design, inherited from the 1973 Xerox Alto, and we need to get past it.
Monday, 14 September 2015
Mouse Marksmanship
 I'm going to have a little rant now. Apologies to all!
WHY do our computers still require "mouse marksmanship"? You know the problem: where you have to spend ages waving the cursor around and over a thin line of pixels, until the cursor finally changes to a double-headed arrow, and you can grab and drag the item - perhaps a wall between two panes in a program's window. Or where there are several tightly-packed buttons and, unless you're accurate, you click the wrong one...with disastrous effects?
Touch-screen interfaces are no better. In fact, they're worse, since fingers are even less accurate than mice or trackpads, and - worse still - they obscure the user interface (UI) elements they're supposed to be interacting with!
I mean...seriously...why is this still a thing? We're perfectly capable of designing operating system interfaces, and applications, that can make sensible guesses as to the user's intention. We can create UI elements that don't need this kind of fine movement requirement - frustrating even to regular users; literally impossible for some to use.
"Mouse marksmanship" makes the whole thing hostile to anyone with a hand tremor, anyone with co-ordination issues or some classes of disability, anyone with even moderate visual difficulties - and everyone else, too.
It's just crap. It's decades-old design, inherited from the 1973 Xerox Alto, and we need to get past it.
I'm going to have a little rant now. Apologies to all!
WHY do our computers still require "mouse marksmanship"? You know the problem: where you have to spend ages waving the cursor around and over a thin line of pixels, until the cursor finally changes to a double-headed arrow, and you can grab and drag the item - perhaps a wall between two panes in a program's window. Or where there are several tightly-packed buttons and, unless you're accurate, you click the wrong one...with disastrous effects?
Touch-screen interfaces are no better. In fact, they're worse, since fingers are even less accurate than mice or trackpads, and - worse still - they obscure the user interface (UI) elements they're supposed to be interacting with!
I mean...seriously...why is this still a thing? We're perfectly capable of designing operating system interfaces, and applications, that can make sensible guesses as to the user's intention. We can create UI elements that don't need this kind of fine movement requirement - frustrating even to regular users; literally impossible for some to use.
"Mouse marksmanship" makes the whole thing hostile to anyone with a hand tremor, anyone with co-ordination issues or some classes of disability, anyone with even moderate visual difficulties - and everyone else, too.
It's just crap. It's decades-old design, inherited from the 1973 Xerox Alto, and we need to get past it.
Monday, 1 June 2015
HPV Vaccination Risks, Versus Cervical Cancer

(Wikimedia Commons)
- All childhood vaccinations other than HPV are given to both sexes equally;
- The takeup rates of all childhood vaccinations are approximately equal, including HPV;
- Reporting rates for adverse reactions are approximately the same for each type of vaccination.
Thus, the cohort size for any given first-five-years vaccination will be approximately double that of HPV (as this is a single-sex vax). Given the variations in diphtheria-type vaccinations (particularly given that some of these are administered in adulthood as top-up or travel vaccinations), I propose to compare MMR (very specifically a first-five-year vax) and HPV.
Scaling appropriately for gender, this gives HPV a 10.3-times greater adverse reaction rate than MMR over the ten year period measured. And of these adverse HPV reactions , 31.4% are classed as "serious".
However, this tells only part of the story. HPV vaccination for schoolgirls was only introduced in 2008, with a catch-up campaign to try to vaccinate older schoolgirls starting a year later. Thus, the HPV cohort is actually likely to be smaller than that of MMR (even given the MMR scares), and the adverse reaction ratio proportionately higher. I can't quantify these, as I don't have figures.
It's clear that the adverse reaction rate is high enough to be of concern. That said, the concrete figures equate to an averaged rate of around 1,000 per year of HPV vaccination (taking into account an estimate of the catch-up uptake rate), giving a serious-reaction rate of around 300 per year. Although that looks high, the number of 12-year-old girls in secondary education in England alone in 2013¹ was about 285,500.
I don't know what the HPV vax uptake rate actually is. I also don't know what the ratio of English schoolgirls to UK-total schoolgirls is. For convenience, let's say the two ratios are about the same - I suspect they're pretty similar - so we appoximate that the cohort size is 285,500.
Based on the above figures, that makes (for HPV) the adverse-reaction rate 0.35%, and the serious-reaction rate 0.10%.
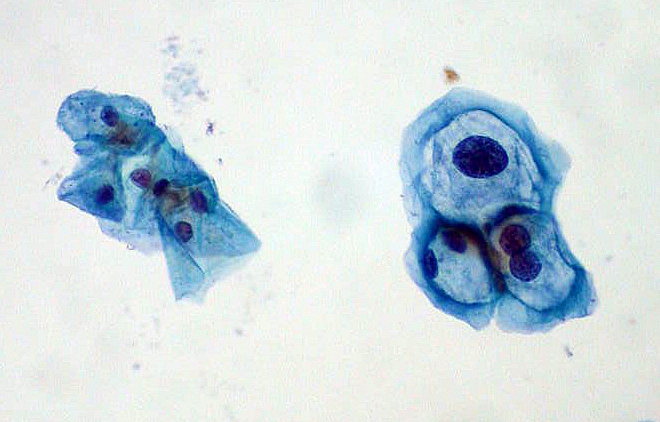
HPV infection smear
Wikimedia Commons
The morbidity rate from HPV vaccination has not been reported, but will be tiny compared to even the severe-reaction rate, otherwise ther would have been a media storm.
My reading of these numbers is that the death risk from vaccination is orders of magnitude lower than that from cervical cancer. So, on the basis of comparison of death risks - and on the assumption that vaccination protection lasts long enough to make a significant difference to cancer incidence rates, vaccination is highly advisable.
If we draw a comparison on harms to health between severe vaccine reactions and incidence (but not morbidity) of cancer, and using the same assumptions as above, the risk from cancer is still substantially (i.e. a substantial multiple) higher than that of vaccine reacting. Hence, vaccination on this basis is very advisable.
Note that I have constrained myself to purely the cervical cancer risks here. HPV vaccination - again assuming its protection is sufficiently long-lasting - also offers protection against a number of other cancer-related and non-cancer-related risks.
¹ https://www.gov.uk/government/statistics/schools-pupils-and-their-characteristics-january-2013
² http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer

